|
|
 | |
Pneumothorax, collapsed lung, or collapsed
chest
|
 |
Normal |
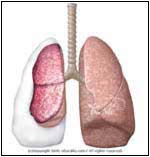
Abnormal |
|
- The lungs are covered by
a saclike membrane known as the pleura, which separates the
lungs from the chest wall (ribs). The pleurae have two layers: one
covers the lungs (visceral), the other is attached to the
inside of the chest cavity (parietal). Between the two
layers there is a thin film of fluid that lubricates the
lungs, allowing them to move smoothly during respiration
(breathing). Under normal conditions, there should be no air
between the lungs and the chest cavity. The introduction of
air into this cavity will cause the lung to collapse, and
compromise breathing.
- The air may leak from a cut or hole in the visceral pleura (i.e., lung problem) or in the parietal pleura (i.e., bullet or knife wound). When air enters the chest cavity, the condition is known as Pneumothorax (p.).
|
 |
- Depends on the size of p.
- Chest pain:
- Sudden
- Sharp or stabbing
- Chest tightness
- Made worse by breathing or coughing
- Shortness of breath
- Cyanosis or bluish color to the
skin and lips due to hypoxia (low oxygen level)
- Rapid rate of breathing
- Fatigue
- Wheezing
- Anxiety
- Patient may be in Shock or unconscious, especially with trauma or tension p.
|
 |
- Primary p. -- in healthy
individuals this occurs without any underlying diseases
- Secondary -- complication of
underlying lung disease
- Spontaneous p. -- often occurs
after the rupture of a bulla (a.k.a bleb) or blister (not
found in normal lungs), which are small air-filled sacs in
the lungs of individuals with certain risk factors. Could be
primary or secondary.
|
 |
- Symptoms
- Injuries
- Procedures or surgeries
- Illnesses
- Medications
- Habits
- Occupation
- Allergies
- Skin may show the site of trauma
- Low Blood Pressure
- Fever may be present
- Cyanosis
- Air can leak under the skin (subcutaneous Emphysema) and has
a spongy feel
- Pallor -- pale skin
- Rapid heart and respiration rate
- The chest movements are not
symmetrical
- The trachea (major airway -- located
in the center of the neck) may be shifted in tension p.
- When the doctor listens to the
heart or the lungs, the normal sounds may be diminished or
absent.
- Chest X-Ray will show the abnormal air pocket, and Collapsed Lung or
structures that have been pushed to one side.
- CAT scan, using computer imaging,
shows detailed views of the chest and lungs.
- Blood tests may show low oxygen
levels (<80 mm Hg) and acidic blood (acidosis = pH
<7.35).
|
 |
- Tall thin males in their 20-40s
(Marfan's and Ehlers-Danlos syndromes)
- Family history of p.
- History of p. -- 50% chance of
recurrence after one episode
- Cigarettes
- Asthma
- COPD (chronic obstructive pulmonary disease) or Emphysema
- Histiocytosis
- Cystic Fibrosis
- Whooping Cough
- Tuberculosis
- Cancer
- Rapid climbing to high altitudes
or while scuba diving
- Pneumonias such as
with Klebsiella or Staph. aureus
- Traumatic -- injury to the chest such as in knife or gunshot wounds, automobile accident, procedures like pleural biopsy, endoscopy, Thoracentesis,
chest tube placement
- Tension p. -- the air is trapped and
builds up with each breath. It can put pressure on and
shift other structures in the chest, such as the
esophagus, trachea, heart, and blood vessels.
- Tension p. risk factors -- lung
infections, trauma to the chest, mechanical ventilation (a
machine that breathes for the patient), and CPR.
|
 |
- Outpatient treatment -- if there is no
hypoxia (reduction of oxygen supply to tissues) and the
collapse is less than 30%:
- Rest
- Assurance that air will be absorbed
into the body without special treatment
- Oxygen therapy
- Monitor blood pressure, heart rate and breathing
- In patient with severe symptoms and
collapse >30%:
- Objective is to remove the air.
- General physician may consult
with a surgeon or a pulmonologist (lung doctor).
- A needle may be used to remove
the air.
- Aspiration involves inserting a catheter (Teflon tube) into the chest cavity (between the ribs) and attaching to a simple bottle (vacuum inside with no air). This may be enough to expand the Collapsed Lung.
- A plastic chest tube is inserted through an incision in the chest (between the ribs) and then connected to suction. This method may take few days to drain the trapped air and expand the Collapsed Lung.
- Multiple episodes of Pneumothorax may
require surgery or injection of medicines (talc or
Doxycycline) into the pleural
space.
|
 |
-
Contact 911 and seek immediate medical attention. If you've had previous episodes, Quit Smoking and talk
to your doctor before high altitude climbing, flying, or
scuba diving.
|
| | |
If you want your friend to read or know about this article, Click here
 |
|
|

